A Deeper Dive into Cardiac Electrophysiology, Autonomic Control, and Pulmonary Defense
Pediatric sedation: Key insights on cardiac electrophysiology, autonomic control, and pulmonary defense to ensure safer dental procedures.
Dental sedation isn’t merely about keeping patients comfortable during procedures—it’s about understanding the intricate physiological systems that ensure their safety. For dental professionals, especially those treating pediatric patients, a thorough grasp of cardiac and pulmonary physiology can make all the difference in managing sedation effectively. In this blog, we take a fresh perspective on key topics such as cardiac electrophysiology, the balance of autonomic control, and the essential role of pulmonary defense mechanisms. These insights, drawn from one of the expert modules in our comprehensive Pediatric Endorsement Sedation Course, provide practical knowledge that can enhance your clinical practice.
The Heart’s Electrical Symphony
At the core of our discussion lies the heart’s remarkable electrical conduction system. The journey begins at the sinoatrial (SA) node, which acts as the natural pacemaker, setting the rhythm for each heartbeat. This impulse swiftly travels to the atrioventricular (AV) node, which introduces a critical delay to ensure that the atria have enough time to empty blood into the ventricles. The signal then travels through the bundle branches and Purkinje fibers, orchestrating a synchronized contraction that efficiently propels blood throughout the body.
Understanding the phases of the cardiac action potential is essential in dental sedation. The process involves a rapid depolarization phase followed by a brief initial repolarization, a plateau phase maintained by the balance of calcium influx and potassium efflux, and finally, a rapid repolarization phase. These phases determine the timing and strength of the heart’s contractions. During sedation, drugs or stress-induced increases in heart rate can alter these phases. For instance, if the heart beats too rapidly, there might not be sufficient time for the ventricles to fill properly, potentially compromising cardiac output and tissue oxygenation. Recognizing these patterns can help practitioners monitor and respond to any adverse cardiac events during sedation.
Balancing Act: Autonomic Control in Sedation
The heart’s function is not solely dictated by its intrinsic electrical system; it is also finely tuned by the autonomic nervous system (ANS). The ANS is divided into two branches: the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS). The SNS acts as the gas pedal, accelerating heart rate and increasing blood pressure in response to stress or emergencies. Conversely, the PNS functions as the brake, reducing heart rate and promoting a state of calm.
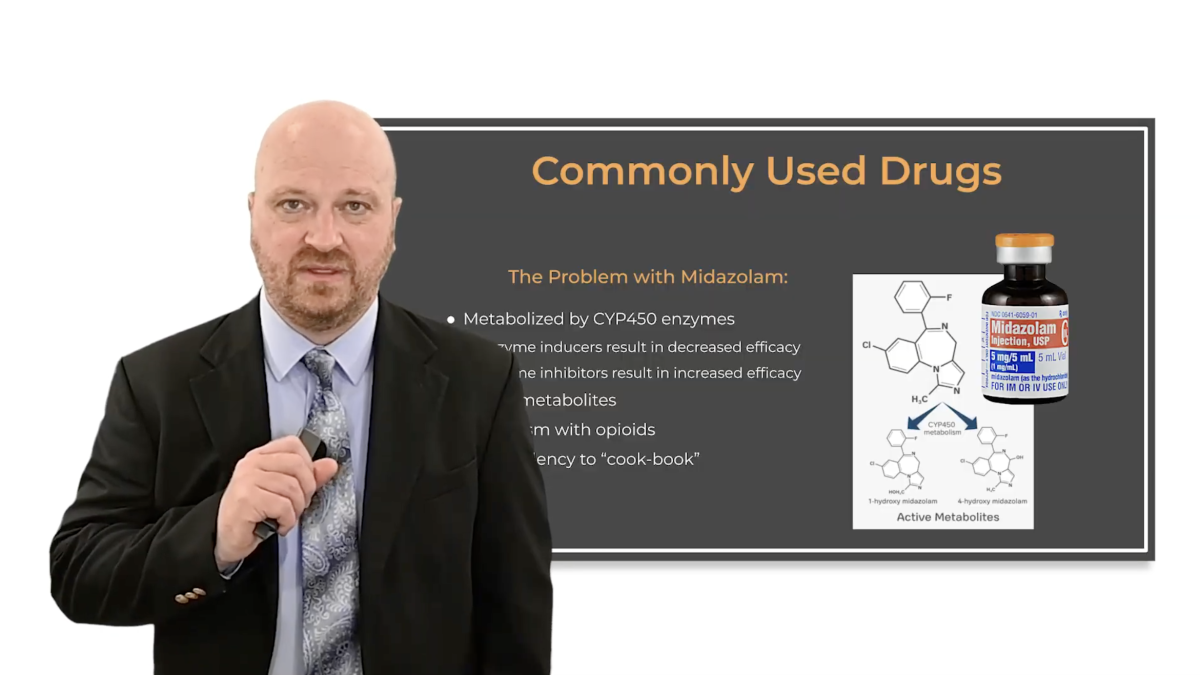
This balance is particularly crucial during sedation. Sedative agents, such as opioids and benzodiazepines, can blunt the body’s natural responses—altering how the heart and lungs react to changes in blood chemistry, such as rising levels of carbon dioxide. For pediatric patients, whose autonomic responses can be more variable, any imbalance may lead to significant changes in heart rate or blood pressure. Dental professionals must, therefore, remain vigilant, adjusting sedation protocols as needed to maintain this delicate equilibrium and ensure patient safety.
Pulmonary Defense: More Than Just Gas Exchange
While the heart’s rhythm and autonomic control often steal the spotlight, the lungs perform equally vital functions, not only in gas exchange but also in protecting the body from airborne hazards. The alveoli, tiny air sacs where oxygen and carbon dioxide are exchanged, are supported by an extensive network of capillaries that ensure efficient oxygen delivery. However, the lungs are more than just passive exchange surfaces—they are equipped with defense mechanisms that keep them clear of debris and pathogens.
Mucus secretion, ciliary movement, and the activity of alveolar macrophages all contribute to a robust pulmonary defense system. During sedation, these mechanisms are especially important. For instance, if a patient’s breathing becomes depressed, the risk of mucus accumulation or aspiration increases. Continuous monitoring of ventilation using devices such as capnographs ensures that any disruption in gas exchange is detected early, allowing for prompt intervention. This vigilance is crucial in pediatric sedation, where even minor disturbances in respiratory function can have significant consequences.
The Safety Net of Lung Volumes
Another critical concept in sedation is functional residual capacity (FRC)—the volume of air that remains in the lungs after a normal exhalation. This “safety reservoir” of oxygen is pivotal during sedation because it sustains the body if breathing temporarily ceases. In pediatric patients, FRC is naturally lower than in adults, making pre-oxygenation a vital strategy before administering sedation.
By increasing the FRC, dental professionals can extend the window of safety during which oxygen levels remain stable, even if the patient’s spontaneous breathing is compromised. Factors such as patient positioning also influence FRC; for example, lying flat or having a higher body mass can reduce this reserve. Understanding these dynamics not only informs better patient management during sedation but also helps in tailoring pre-sedation preparations to optimize safety.
Putting It All Together for Better Sedation Outcomes
Incorporating knowledge of cardiac electrophysiology, autonomic control, and pulmonary defense into your sedation practices can significantly enhance patient safety and outcomes. Each of these systems plays a critical role during sedation, and their interrelationships determine how well a patient tolerates a procedure. A rapid heart rate can shorten diastole, reducing ventricular filling and oxygen supply, while altered autonomic balance can predispose a patient to dangerous fluctuations in heart rate and blood pressure. Similarly, an understanding of lung volumes and pulmonary defense mechanisms is essential for managing the respiratory challenges that can arise during sedation.
This comprehensive understanding allows dental professionals to anticipate complications and adjust their sedation protocols accordingly. Whether it’s modifying drug dosages, optimizing patient positioning, or employing advanced monitoring technologies, the insights gained from this module can help refine your clinical approach and elevate your standard of care.
Elevate Your Sedation Practice with Expert Training
The insights presented in this module—developed by Dr. Bryant Cornelius—offer just a glimpse into the depth of knowledge available in our Pediatric Endorsement Sedation Course. Dr. Cornelius is one of several expert instructors leading this comprehensive program, designed to equip you with the skills and practical strategies needed to manage pediatric sedation safely and effectively.
The course provides 16 CE credit hours and covers a broad spectrum of topics including sedation pharmacology, patient management, emergency protocols, and pre- and post-sedation procedures. By enrolling, you’ll gain access to expert insights from a dedicated team of professionals committed to advancing the standards of pediatric sedation practice.
If you’re ready to take your expertise to the next level and ensure the highest quality of care for your young patients, we invite you to enroll today. Visit isedatesafe.com to secure your spot in the Pediatric Endorsement Sedation Course and join a community of dental professionals dedicated to excellence in sedation.
 Sani Leauanae
Sani Leauanae