Pre- and Post-Sedation Procedures: Risk Management, Informed Consent, and Safety Protocols
Understanding Dental Sedation: A Comprehensive Overview for Professionals
Sedation is an essential part of modern dentistry, especially when treating pediatric and adolescent patients. Administering sedation safely requires a deep understanding of not only the pharmacology involved but also meticulous documentation, risk management, and patient care. In this blog, we’ll explore the critical aspects of dental sedation, including patient evaluation, informed consent, sedation equipment, and the importance of procedural monitoring. This guide will provide valuable insights for dental professionals seeking to enhance their knowledge and practice of dental sedation.
The Importance of Dental Sedation
Dental sedation offers significant benefits for patients with high levels of anxiety, those undergoing lengthy procedures, and patients who have trouble staying still during treatment. Proper sedation ensures that the experience is more comfortable for the patient and allows dentists to perform their work more efficiently. However, administering sedation comes with the responsibility of managing risks and adhering to protocols to ensure patient safety.
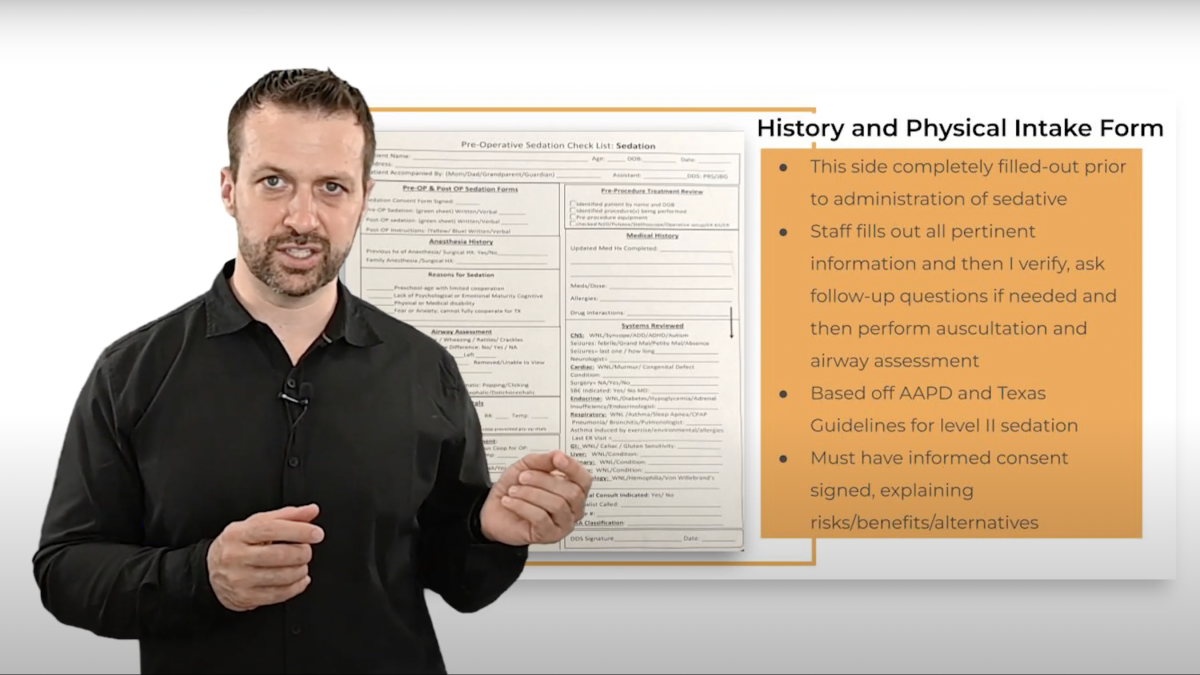
Patient Evaluation and Pre-Sedation Checklist
Before administering any sedative agent, conducting a comprehensive patient evaluation is paramount. This initial step serves to ensure that patients are fit for sedation and helps identify any medical conditions that might complicate the procedure. Patient evaluation begins with documenting their ASA (American Society of Anesthesiologists) classification, reviewing their medical history, and confirming medications being taken.
For patients classified as ASA 3 or 4—indicating more significant health concerns—medical clearance from their primary care physician or a specialist is required before sedation can be administered. This precaution ensures that all potential risks have been evaluated and that the patient is in a stable condition for sedation.
Informed Consent: Setting Expectations and Managing Risk
Informed consent is a critical component of dental sedation, where patients or their guardians must be fully aware of the risks associated with the procedure. This includes the potential for serious complications such as cardiac arrest, brain injury, or even death in extreme cases. It’s essential to provide the informed consent in written form, where the patient or guardian signs off on the sedative agents to be used, the procedure itself, and any risks involved.
A thorough explanation before the procedure can prevent confusion and miscommunication during the process. An informed consent form should also cover instructions regarding NPO (nothing by mouth) guidelines and any pre-procedure preparations. It's crucial to remember that patients and their guardians can withdraw their consent at any time, even during the procedure. Therefore, ensuring they fully understand the implications of the treatment is vital for maintaining trust and providing a positive dental experience.
Equipment and Monitoring: Safety Protocols in Place
Adhering to safety protocols is a must when dealing with sedation. The Texas Administrative Code outlines essential requirements for sedation procedures, which include ensuring adequate oxygen supply, baseline vital monitoring, and the presence of emergency equipment. Even for minimal sedation cases, it's safer to follow the documentation and monitoring standards for moderate sedation.
Key equipment includes positive pressure oxygen delivery devices, working nitrous oxide alarms, and emergency medications readily accessible in case of an adverse reaction. In addition, continuous monitoring is required throughout the sedation procedure and recovery. This includes regular checks on the patient’s heart rate, blood pressure, respiratory rate, and oxygen saturation levels. Proper monitoring not only helps track the effectiveness of the sedation but also ensures that any signs of distress are immediately addressed.
Procedural Monitoring: Keeping a Close Eye
Monitoring during sedation is one of the most important steps in ensuring patient safety. Regular documentation of vitals, including blood pressure, heart rate, and oxygenation, is crucial. In many dental offices, electronic monitoring systems simplify this process, providing real-time data and timed recordings that can be printed and added to the patient’s chart. However, for those without electronic systems, manual recordings are equally important and should be documented at intervals no longer than ten minutes.
The need for continual verbal communication with patients throughout the procedure, even during sedation, helps evaluate the patient’s level of consciousness and responsiveness. Ensuring that the patient can maintain verbal contact offers additional reassurance that they are sedated at the appropriate level.
Post-Sedation: Recovery and Discharge Protocols
Once the dental procedure is complete, the recovery phase begins. Post-sedation monitoring is crucial as many complications can arise during this stage. The patient must reach a satisfactory level of consciousness and demonstrate the ability to respond to verbal commands before being discharged. Patients should be fully monitored until they are no longer at risk for airway compromise or resedation, which can occur if reversal agents are administered.
The post-sedation recovery phase should also be thoroughly documented. This includes recording final vitals and confirming that the patient has met discharge criteria, such as regaining motor control and being able to sit or stand unassisted. Written instructions should be provided to the caregiver, outlining the necessary steps for post-procedure care, including emergency contacts and follow-up appointments.
In summary, dental sedation plays a vital role in modern dentistry, offering significant benefits for both patients and practitioners. However, sedation must be administered with care, adhering to all pre-procedural, intra-procedural, and post-procedural safety protocols. Proper patient evaluation, informed consent, diligent monitoring, and thorough documentation are the cornerstones of safe and effective dental sedation.
As dental professionals, our responsibility is to ensure that patients are sedated safely and recover smoothly, with minimal risk. Keeping up to date with sedation practices, equipment requirements, and legal obligations is critical for maintaining a high standard of care.
Learn more from the instructor of this course
Dr. Jeff Gregerson, a Board-Certified Pediatric Dentist with over 14 years of experience, has dedicated his career to ensuring the safety and comfort of pediatric and adolescent patients undergoing sedation. With advanced training from the University of Pennsylvania and the Children’s Hospital of Philadelphia, Dr. Gregerson has developed expertise in hospital-based dentistry, sedation, and anesthesia techniques. He currently serves as Co-Chief of Dentistry at Dell Children’s Medical Center and brings his vast knowledge of sedation and patient care to this specialized course.
If you’re a dental professional looking to expand your sedation expertise, Dr. Gregerson’s module on comprehensive pre- and post-sedation procedures is a must. His experience in pediatric sedation, combined with his dedication to patient safety, ensures that you’ll gain valuable insights that can immediately be applied to your practice.
Take the next step in your professional development by enrolling in the Pediatric Endorsement Sedation Course today. Gain 16 CE credits and learn how to safely administer sedation to pediatric patients, meet Texas State Board of Dental Examiners (TSBDE) standards, and enhance the care you provide.
Don’t miss out on the opportunity to learn from Dr. Gregerson and improve the safety and efficacy of your sedation techniques. Expand your skills, meet regulatory requirements, and ensure the highest quality of care for your patients, enroll now.
Categories: : Patient Safety
 Sedation and Anesthesia Education
Sedation and Anesthesia Education