How Understanding the Heart and Lungs Improves Your Sedation Safety
Sedation is one of the most valuable tools we have as dental professionals. It helps patients stay calm, comfortable, and still during procedures that might otherwise be traumatic or intolerable. But for sedation to be both safe and effective, we need a solid grasp of the systems it affects most: the heart and the lungs.
This post breaks down the essential cardiopulmonary physiology every dentist should understand—especially those who administer sedation in their practice.
The Heart Is More Than a Muscle—It’s a Precise Machine
Your heart beats roughly 100,000 times a day. Over the course of a lifetime, it can beat over 3 billion times. And while we often think of it as a single organ, the heart is really two pumps in one: the right side pumps blood to the lungs, and the left side pumps it to the rest of the body.
Each side of the heart has two chambers (atrium and ventricle) and a series of valves that keep blood moving in the right direction. The atria act as primer pumps, sending blood to the ventricles. The ventricles are the strong pumps that do the heavy lifting.
Why does this matter in sedation? Because anything that affects heart rate or the way the heart fills can reduce oxygen delivery to the brain and body. This is especially important when sedatives or anesthetics are in use.
Why Faster Isn’t Always Better
A heart that beats faster doesn’t necessarily pump more blood. In fact, as heart rate increases, the amount of time the heart spends in its filling phase (diastole) decreases. That means the heart fills less completely, and less oxygenated blood is sent to the body. Coronary arteries, which feed the heart muscle itself, are also perfused during diastole—so a fast heart rate can starve the heart of its own oxygen.
This becomes relevant when patients are anxious (as they often are in the dental chair), and especially when we inject epinephrine-containing local anesthetics. If a patient has a borderline heart condition, their cardiac function may not tolerate this extra demand.
The Cardiac Cycle: What’s Happening in Each Beat
The heartbeat isn’t one simple movement. It goes through distinct phases:
- Filling: Blood flows into the ventricles.
- Isovolumetric Contraction: Pressure builds in the ventricles.
- Ejection: Blood is pushed into the aorta or lungs.
- Isovolumetric Relaxation: The heart relaxes before the next cycle.
Understanding these stages helps us interpret vital signs, EKGs, and how certain drugs might influence cardiac function during sedation.
How Cardiac Cells Work Differently
Unlike skeletal muscles, cardiac muscle cells are connected by special structures called intercalated discs. These allow electrical signals to move quickly from cell to cell, which is essential for coordinated heartbeats. The action potential in heart muscle includes a unique plateau phase, due to calcium channels that stay open longer. This prolongs contraction and ensures the heart has time to pump effectively.
This matters when considering how drugs like calcium channel blockers or beta-blockers (and even sedatives) interact with the heart.
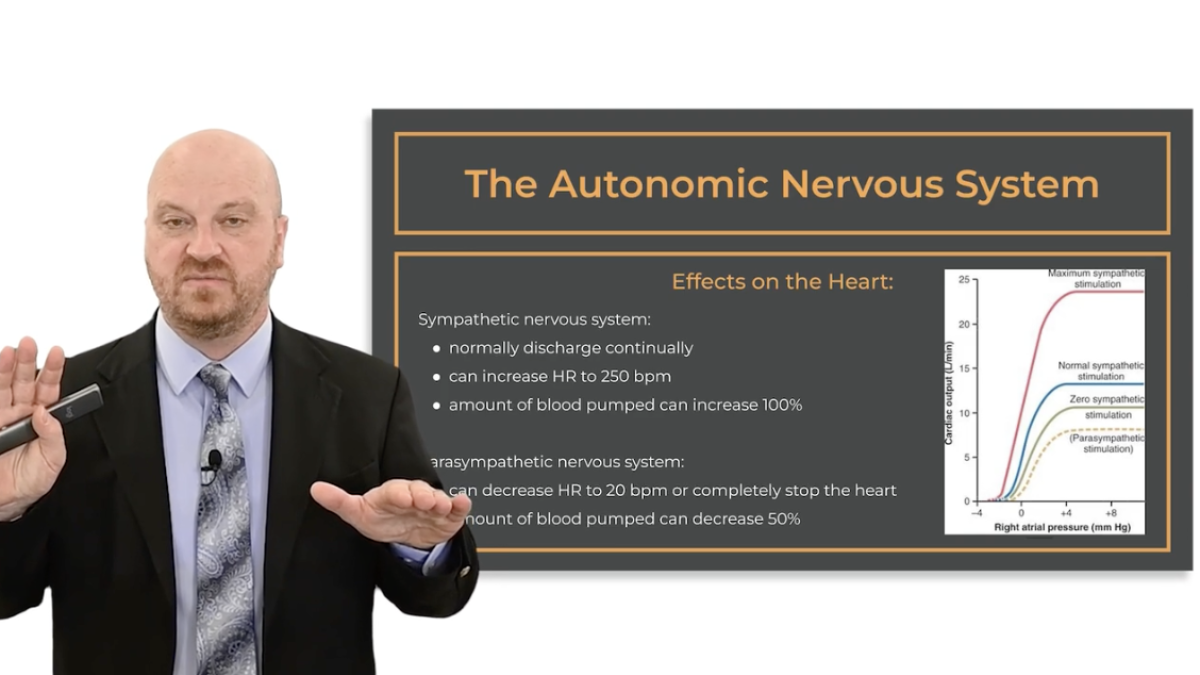
The Nervous System’s Role
Your heart and lungs are under the control of the autonomic nervous system:
- Sympathetic (fight or flight): Speeds things up.
- Parasympathetic (rest and digest): Slows things down.
Epinephrine, for instance, activates the sympathetic system. Atropine, which we might use in emergencies, inhibits the parasympathetic system. Understanding how these systems work—and how the drugs we use affect them—is critical to safe sedation.
The Lungs: Not Just for Breathing
The lungs do much more than bring in oxygen. They also:
- Help regulate the pH of blood
- Metabolize certain drugs
- Remove carbon dioxide (a key driver of breathing)
During sedation, monitoring ventilation is just as important as monitoring oxygen saturation. Devices like capnographs give real-time feedback about CO₂ levels—and can alert you to hypoventilation before pulse oximeters do.
Functional Residual Capacity: Your Safety Net
When a patient stops breathing during sedation, the only oxygen available is the air still left in their lungs—this is called functional residual capacity (FRC). Several things affect FRC:
- Lying flat reduces it
- Obesity reduces it
- Pre-oxygenation increases it
Pre-oxygenating a patient with 100% oxygen before starting sedation can give you several extra minutes to intervene in case of respiratory compromise. That’s a simple step that could save a life.
Air Moves Because of Pressure
Breathing isn’t magic—it’s physics. When the chest expands, pressure inside the lungs drops, and air flows in. During expiration, the opposite happens.
Positive-pressure ventilation (like with a bag-valve mask) works by artificially increasing pressure outside the lungs to push air in. You can’t use it effectively if you don’t understand how air moves—and what your equipment is doing.
So, Why Does All This Matter?
Sedation in dentistry isn’t just about calming a patient. It’s a medical procedure that affects major organ systems. Having a clear grasp of the physiology behind cardiac and respiratory function helps you:
- Predict how your patient might respond to sedation
- Recognize early signs of trouble
- Act faster and more confidently when needed
If you need a refresher or want more hands-on training in emergencies, airway management, and monitoring, check out our Respiratory and Circulatory Physiology for Sedation & Anesthesia.
More sedation training and CE resources available at www.isedatesafe.com
Categories: : Sedation Anesthesia
 Sedation and Anesthesia Education
Sedation and Anesthesia Education