The Heart, the Lungs, and the Drill: What Dentists Should Know Before Sedating a Patient
Most dentists aren’t looking to become cardiopulmonary experts—but if you’re practicing sedation, even at the minimal or moderate level, a working understanding of basic physiology can make the difference between a routine appointment and a case that veers off track.
Sedation dentistry doesn’t fail because the drug dose was wrong. It fails when physiology doesn’t cooperate. When the patient’s heart doesn’t respond predictably. When their lungs don’t keep up. When the numbers on the monitor look “fine”—right up until they don’t.
That’s why we need to talk about the heart and lungs, not from a textbook perspective, but from a dental operatory point of view.
When Faster Isn’t Better: The Heart and Diastolic Fill Time
We often focus on blood pressure and heart rate as simple numbers—"normal" or "abnormal." But what those numbers represent matters, especially during sedation.
Every heartbeat has two phases. Diastole is when the heart relaxes and fills with blood. Systole is when it contracts and pumps that blood out. The issue during sedation is that when heart rate increases—due to anxiety, pain, or epinephrine—diastole shortens more than systole. That’s a problem, because coronary arteries fill during diastole. The faster the heart beats, the less time it has to oxygenate itself.
For the healthy teenager getting third molars removed, that’s not a big deal. But in an adult with hypertension, CAD, or even just a long history of unmanaged stress? The difference matters.
Sedation isn’t just about calming the patient emotionally. It's a physiological intervention that can protect the heart by helping preserve that all-important diastolic filling time.
The Hidden Danger of "Normal" Pulse Oximetry
Pulse oximeters are helpful, but they don’t give us the full story. They show us how much oxygen is in the blood—but not whether the patient is actually moving air. In fact, SpO₂ is a lagging indicator. By the time it drops, the patient may have already been apneic for 30 seconds or more.
This is where capnography comes in. Measuring end-tidal CO₂ gives us real-time information about ventilation. If the patient stops breathing, the capnography waveform flattens immediately—even if their oxygen saturation is still holding. That flat line is your first signal that something’s off.
In the sedation setting, especially when using medications that blunt respiratory drive, capnography isn’t just a safety feature—it’s an early warning system.
Lung Volume and the Reclined Patient
Another piece of this puzzle is functional residual capacity—the amount of air left in the lungs after a normal exhalation. This volume serves as an oxygen reserve during periods of apnea. But when a patient is obese, has sleep apnea, or is fully reclined, their FRC is significantly reduced.
In practical terms, that means they desaturate faster if they stop breathing. They don’t have the same cushion of oxygen that healthier or better-positioned patients do.
For these cases, small adjustments—like keeping the chair slightly elevated or taking a few minutes to preoxygenate—can dramatically increase safety. These are the kinds of preventive decisions that rarely get noticed, unless they’re skipped.
What the Medical History Is Really Telling You
It’s easy to breeze past familiar meds on a health history form. Propranolol, lorazepam, albuterol—they’re common. But each one has implications for sedation.
Beta-blockers like propranolol suppress the sympathetic nervous system. That means your patient may not show a typical rise in heart rate in response to low blood pressure. Benzodiazepines already present in the system can increase the depth and duration of sedation. A rescue inhaler might point to an airway that’s more reactive than the patient lets on.
Medical histories aren’t just about clearance. They’re an opportunity to anticipate how a patient might respond differently under sedation—even when everything else seems routine.
Why Some Patients Don’t Warn You Before They Stop Breathing
Under normal conditions, the body triggers breathing based on carbon dioxide levels—not oxygen. But sedatives, especially opioids and benzos, blunt the brain’s sensitivity to CO₂. That means patients may stop breathing without the usual warning signs—no gasping, no struggling—just silence.
These are the moments where sedation “fails” not because you did something wrong, but because the patient’s physiology changed in a way you weren’t fully expecting.
This is why building your sedation strategy around anticipation rather than reaction is so essential. And that kind of thinking isn’t always taught in CE.
When Sedation Fails, What Comes Next?
Every dentist practicing sedation will, at some point, encounter a case that doesn’t go as planned. Maybe the patient doesn’t sedate deeply enough. Maybe they go too far. Maybe their physiology doesn’t respond predictably. In those moments, success depends on your ability to adapt—quickly and safely.
If you’re looking to sharpen your skills beyond the basics, there's a course that speaks directly to that reality.
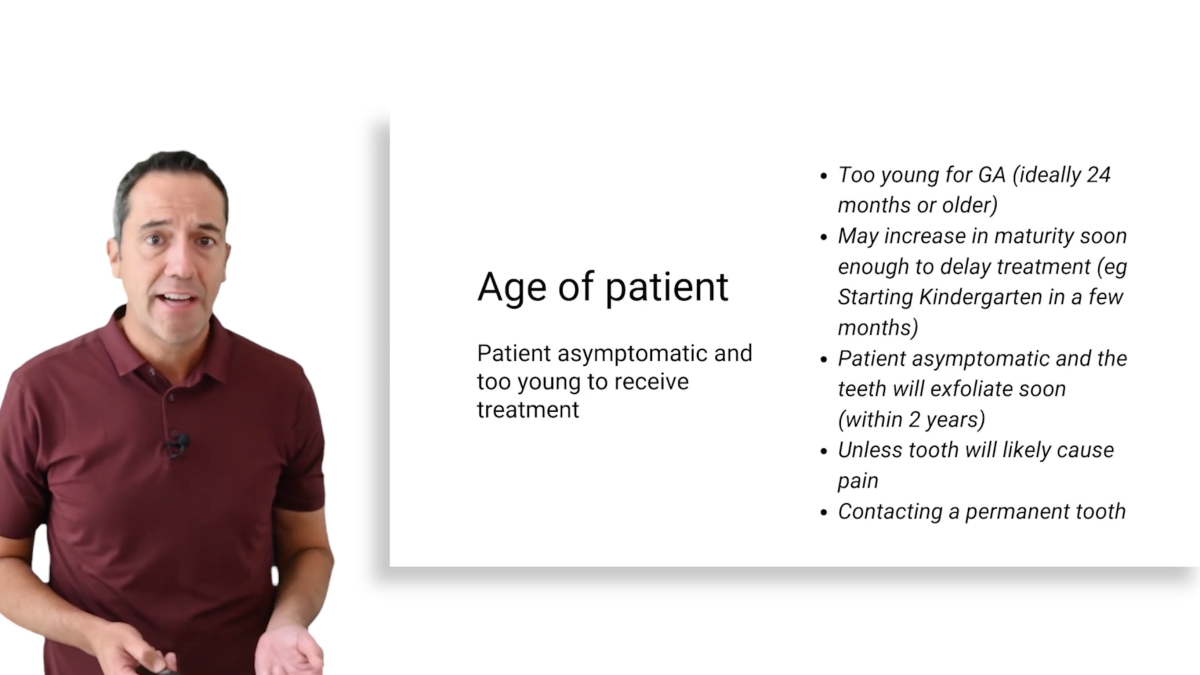
When Sedation Fails: Alternative Strategies & General Anesthesia Considerations is taught by Dr. Stephen Montoya, a board-certified dentist anesthesiologist with decades of experience across private practices, hospitals, and surgical centers. He’s managed hundreds of high-risk cases—and he built this course around what he wished more dentists knew before things got complicated.
It’s not a pharmacology review. It’s not a theory-heavy seminar. It’s a practical guide for general dentists who want to be better prepared when sedation doesn’t go according to plan.
Closing Thought
Sedation dentistry is safer today than it’s ever been—but only if we respect the systems we’re affecting. The heart and lungs might not be your daily focus, but when you sedate a patient, they become your responsibility.
Understanding these systems doesn't just make you a safer provider. It makes you a more confident one.
If you want to build that kind of confidence—and you're ready to move beyond sedation 101—consider taking a closer look at what happens after the protocol fails.
 Akela Leauanae
Akela Leauanae